1 Introduction
Over the past half century, access to mental health services in the United States has expanded, and the quality of services received has improved (1). Growing recognition of the importance of financial access to services and strong support by the advocacy community have led to public policy developments in the past decade that have rapidly accelerated these longstanding trends. Enactment in 2008 of the Mental Health Parity and Addiction Equity Act (MHPAEA) expanded financial access to treatment for mental and substance use disorders among individuals with private insurance. Provisions in the Affordable Care Act that established mental health and substance abuse services as required elements of the essential health benefit, in combination with MHPAEA, further extended these insurance protections. The expansion of Medicaid, the introduction of insurance subsidies for near-poor Americans, and reform of the individual and small-group health insurance markets meant that a growing share of the population gained access to this improved coverage.
In total, over the past decade, some 174 million Americans either obtained coverage for mental and substance use disorders for the first time or had their existing coverage become more complete (2). This has translated into reduced financial barriers to treatment (3), expanded use of mental health and substance use treatment among children and youth, infusion of billions of dollars into the care of low-income individuals with mental and addictive illnesses (4), and reduced levels of psychological distress in low-income populations residing in states that expanded Medicaid (5; and authors’ tabulations of data from the National Health Interview Survey).
These substantial improvements in financial access to treatment, however, have been accompanied by a growing recognition that access to treatment is not enough to significantly improve the lives of individuals with the most serious mental illness. In particular, access to treatment alone has not accomplished much with respect to the broader goal of integrating those with the most serious mental illnesses into our communities. Even as treatment access has improved, participation in the workforce of persons with serious mental illness has stagnated. For many persons with mental illness, active participation in the workforce is a critical aspect of community integration and of recovery (6).
The challenge of integrating individuals with serious mental illness into the community and workforce has long been recognized. And there is good reason to believe that despite improvements in treatment, that challenge is becoming more difficult. Even as access to care has improved, the economy itself has changed. The 21st century labor market demands a different set of skills from the workforce. Automation of routine tasks has been accelerating, and the use of industrial robots has tripled from 2008 to 2017 (7). Technological improvements in information and communications technology demand a workforce that has the capacity to engage in non-routine, cognitive-intensive work (8). These technological trends displace low-wage jobs and jobs that require the ability to perform routine cognitive and non-cognitive tasks (9). This pattern of changes in workforce needs may have profound effects on the employment prospects for people with mental illnesses. In this paper, we argue that the evolution of the U.S. labor market poses critical challenges for people with mental illnesses, because the changing nature of work may narrow opportunities for individuals who experience the cognitive impairments that are associated with a number of major mental illnesses. These developments coincide with new approaches to treating serious mental illnesses that are oriented toward preventing disability and supporting continued attachment to the labor market. Our existing policy infrastructure has not yet incorporated either these changing trends in workforce demand or these new approaches to treatment. We conclude with suggestions for how policy can promote continued attachment to work for people with mental illnesses.
2 Mental Illness, Human Capital, and Skill Development
A number of the most prevalent mental illnesses lead to significant cognitive dysfunction. A recent review summarized evidence for cognitive dysfunction in seven categories of mental illness (10). The reviewers concluded that for many people with mental illness, “cognitive dysfunction is broad based and seriously affects real-world functioning.” More specifically, they showed that major depression, bipolar disorder, schizophrenia, obsessive-compulsive disorder, and posttraumatic stress disorder have important impacts on attention, working memory, executive function, processing speed, and social cognition. These cognitive dysfunctions, along with some of the motivational and affective features of mental illnesses, translate into impairments in skills that are known to affect productivity, such as concentration, problem solving, communication, organization, adaptability, and collaboration. Thus, cognitive dysfunctions pose serious challenges to labor market activity for people with mental illnesses. The challenges are exacerbated by the fact that the onset of a number of these illnesses is in late adolescence and early adulthood. Early onset means that these conditions can compromise the accumulation of human capital in the forms of education, training, and job experience, leaving people with these illnesses at a lifelong disadvantage. The probability of graduating from high school, entering college, and completing college are each about two percentage points lower among persons with a mental illness that began in childhood or adolescence than among those without evidence of an early-onset mental illness (11).
These clinical sequelae of mental illness are consistent with the observable labor market experience of people with mental disorders. Many years of research have documented that individuals with mental disorders are more likely to leave the labor market than are those without these conditions, they also earn less, are disproportionately employed in low-skill occupations, and have high rates of poverty. Table 1 shows the ratio of employment rates for persons with severe and moderate mental illnesses compared with rates for persons without any diagnosable psychiatric conditions. Mental illness is associated with reduced rates of full-time work (62% to 83% as high as rates for those without a mental illness), increased part-time work, and higher rates of being out of the labor force (1.58 times as high and 2.05 times as high for those with moderate and severe illnesses, respectively). Similar findings have been reported by Luciano and colleagues (12).
Table 1 / Supplemental Security Income Enrollement for Mental Disorders
Source: National Household Survey on Drug Use and Health 2013-2015

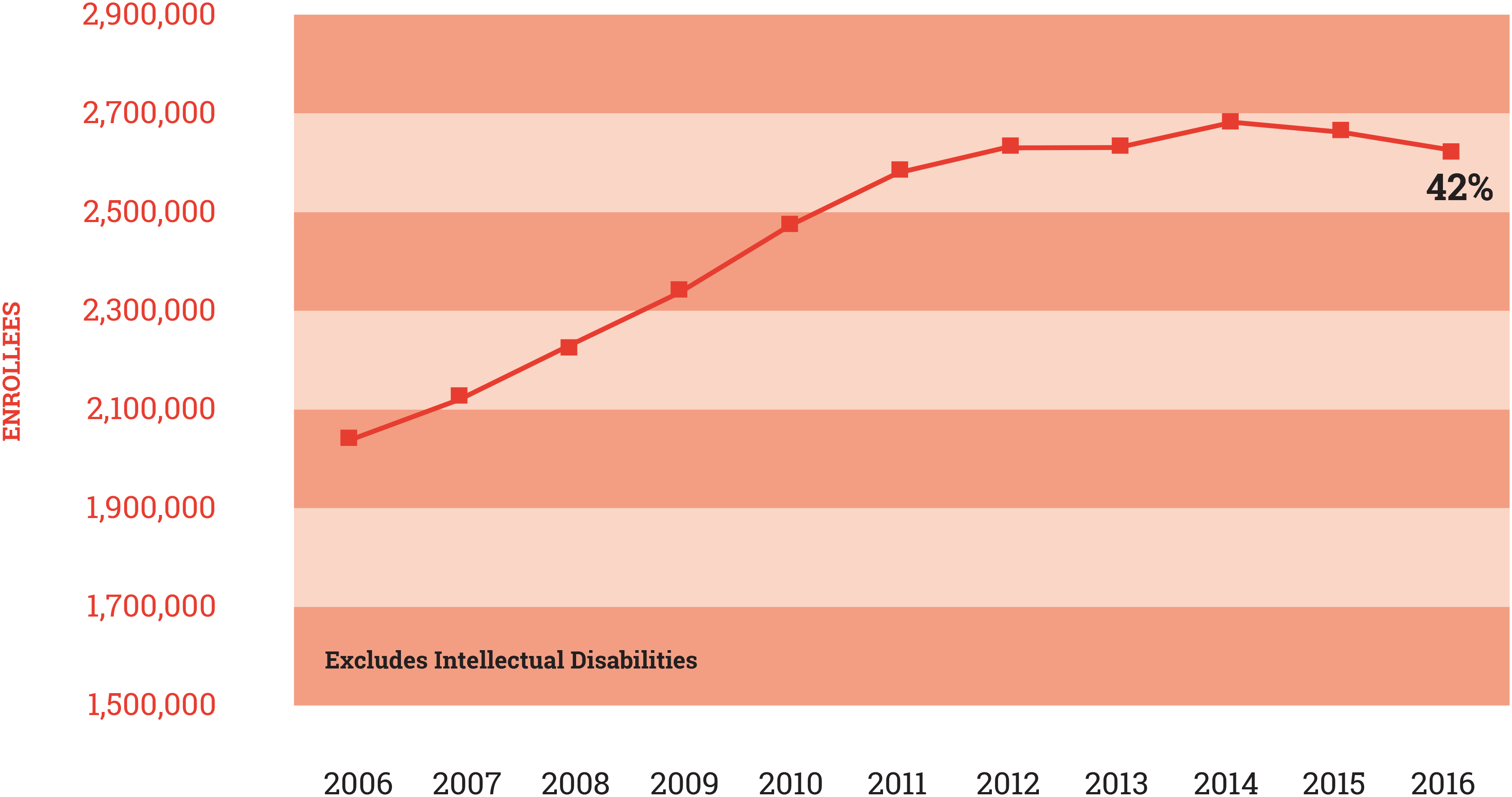
Across a broad range of diagnoses, people with serious mental illnesses are estimated to earn on average only 69% as much as the general population. Those with moderate mental illnesses earn about 91% as much (13). The early onset of mental illnesses, combined with their lifetime disruptive effects, help to explain why people with mental illnesses are more likely to work in low-skill occupations in all high-income countries (13). These poor employment outcomes mean that between 25% and 32% of people with a serious mental illness live on incomes that are below the federal poverty line (authors’ tabulations of data from the National Survey on Drug Use and Health and the American Community Survey), a rate more than twice as high as the average U.S. populations rate of 12.7% in 2016 (14). Finally, mental illnesses are the cause of relatively large numbers of claims on disability programs. Figure 1 shows the trend in enrollment in the Supplemental Security Income program. Since 2006, enrollment by people with mental illnesses has increased by about 28%, and this group now accounts for 42% of program enrollees.
In sum, evidence shows that mental illness has contributed to diminished employment and earnings and consequently to high rates of poverty among people with serious mental illnesses and to high levels of participation in public programs for individuals disabled by mental illnesses. This disconnection between mental illness and productive employment is likely to become worse in the future.
Figure 1 / Supplemental Security Income Enrollement for Mental Disorders
Source: Authors’ tabulations of data from the National Survey on Drug Use
3 The 21st Century Labor Market: Challenges for People with Mental Illnesses
The 21st labor market increasingly favors individuals who have a post-secondary education and specific types of skills. Between 2007 and 2016, the number of U.S. jobs that required no more than a high school education declined by 1.3 million. Over the same period, the number of jobs that required at least some post-secondary education increased by 5.3 million (15). The Bureau of Labor Statistics of the U.S. Department of Labor projects that this trend will accelerate. Between 2016 and 2026, it predicts that the number of jobs requiring a master’s degree will grow by 15.8%, those requiring a bachelor’s degree will grow by 10%, and those requiring only a high school diploma will grow by just 5.2% (16).
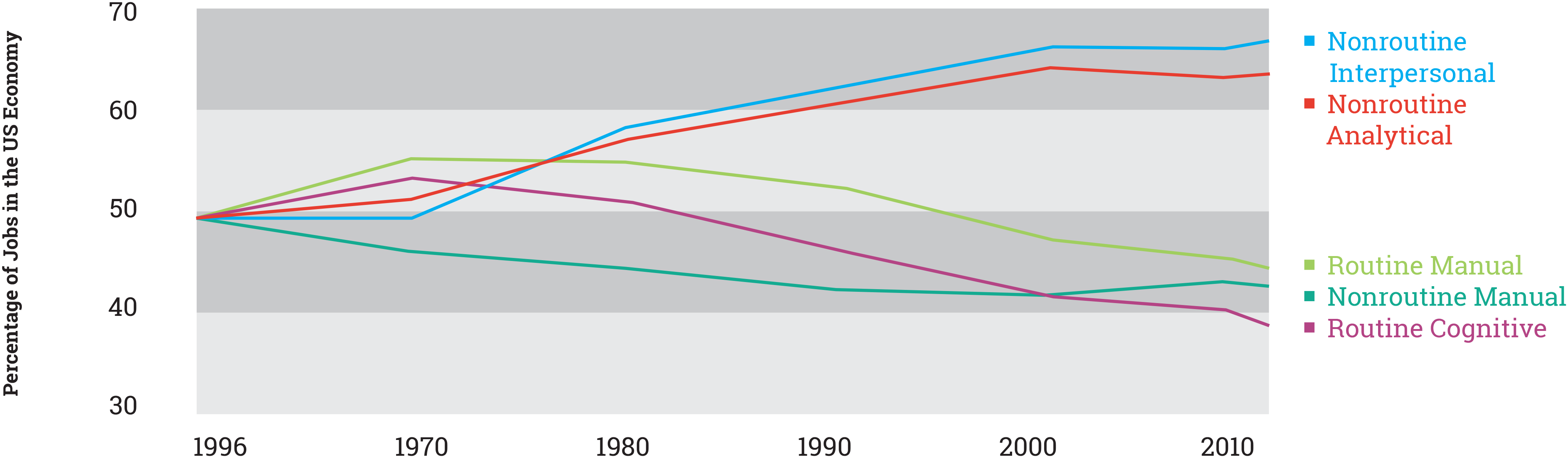
This growing demand for post-secondary education parallels a shift in the types of skills being sought by employers. Figure 2 reproduces a graph of the changing skill mix in the U.S. economy originally published by the World Economic Forum (9). The illustrated trends in skill mix show that the world economy has increasingly demanded—and is likely to continue to demand—more employees with non-routine interpersonal and cognitive skills and fewer employees with manual and routine cognitive skills. The graph highlights that the demand for employees with routine cognitive and manual skills has fallen 20% since 1980 while the demand for workers with non-routine cognitive and interpersonal skills has increased by 17%. These patterns of demand for education and skills complement the data on labor market outcomes described above. The combination of impairments in cognitive functioning, the likely interpersonal affects resulting from those impairments, and recent trends in labor demand explains why opportunities for employment of people with major mental illnesses have not improved with access to treatment and may even be in decline.
Figure 2 / Distribution of Skillsets in U.S. Labor Market
Source: Data provided by David Autor at MIT and updated from the original 2003 study by Autor, Levy, and Murnane.
Forecasts of trends in employment coupled with our understanding of the nature of the impairments associated with mental illnesses make clear that the very skills for which demand is growing are those that mental illnesses are most likely to affect. Moreover, individuals with mental illnesses are likely to be further affected by intensifying competition for the remaining employment opportunities that require more routine cognitive and manual skills (17). Persons with mental illnesses are likely to fare poorly in this more competitive market, due in part to their potentially lower productivity but also to the stigma that continues to be attached to mental illnesses.
In sum, if we are to make progress in social integration and greater engagement in work of people with serious mental illnesses, then it is important to anticipate emerging trends and develop policy and programmatic responses that will maximize opportunities for these individuals. In addition, the policy and programmatic responses that are likely to work best in the face of these expected trends will also yield immediate benefits.
4 Policy Responses
We consider three broad types of policy responses to the emerging challenges we have documented:
- Continued efforts to develop and diffuse early intervention programs
- Creation of better incentives for employers to invest in programs that accommodate workers with mental illnesses
- Investment in technologies that can support people with mental illnesses in the workplace.
There is new optimism in the mental health field with respect to the potential to affect disability from serious mental illnesses (18). The evidence to date suggests that programs that make use of supported employment arrangements within a program of early intervention in schizophrenia, such as those in the RAISE trial, result in greater engagement in work activity and higher levels of social integration (19). These positive findings, however, are tempered because these programs have, at least to date, shown little or no significant impact on disability rates and no meaningful effect on earnings.
The RAISE trial (Recovery After an Initial Schizophrenia Episode) showed that intervention can help, but it also underscored the importance of earlier identification and engagement of patients to increase the effectiveness and cost-effectiveness of treatment and supported employment (20). Although RAISE was targeted at first-episode cases and effects were greatest among those early in the course of illness, many individuals who participated in the intervention had been symptomatic for a considerable length of time. The median duration of untreated psychosis in the trial was 74 weeks, and the mean was over 178 weeks (18). If first-episode treatment and supported employment are to reduce disability, additional steps will be needed to accelerate identification and engagement of persons in need of services. The Demonstration to Maintain Income and Employment (DMIE), a more recent trial, offers promising clues for targeting the interventions of the RAISE program to generate the largest potential effects. DMIE showed that intervening in earlier stages of mental illness, when people are still working, produced meaningful impacts on disability program participation (21). In sum, a promising strategy for translating treatment gains into gains in employment and inclusion is to target early intervention programs, including supported employment, to those in the initial stages of illness. Early intervention will help people today and will be of even more importance as the demand for labor changes.
Early intervention provides an external scaffold for people with mental illness in the labor market. A second set of policies we consider focuses on enhancing opportunities for people with mental illness within their jobs by increasing incentives and opportunities for employers to accommodate and support these workers. Under the Americans with Disabilities Act (ADA) of 1990, employers are prohibited from discriminating against current or potential employees because of a disability and must provide reasonable accommodation for people with a disability, if these are not excessively costly. Unfortunately, courts have interpreted the ADA to limit protections for workers whose illnesses are controlled through medications. Further rulings have extended this exemption in ways that make it challenging for people with mental illnesses to successfully claim protections (22). By explicitly extending the protections of the ADA to people with mental illnesses, Congress would create incentives for employers to develop and implement appropriate and inexpensive accommodations. Although prior research suggests that features of such accommodation might include using flexible work schedules, breaking jobs into sub-components, and providing more explicit instructions for tasks, new technologies might make these and other accommodations more effective and practical (23). In effect, this would advance an argument that the standard for accommodation of mental illness ought to be at parity with that for comparably costly physical illnesses.
Another vehicle for increasing employer incentives is to extend the protections of employer-provided long-term disability insurance programs. In 2013, only about one-third of employers provided access to such programs, and benefits under these programs were often lower for mental than for general medical illnesses. Policy analysts who are focused on disability more generally have advocated requiring employers to provide such protections to all their employees (24). Requiring more employers to offer such benefits and extending parity to these programs has two benefits. First, it would provide more income protection to people with mental illness who are unable to work. But even more important, it would give employers strong incentives to accommodate their employees’ illnesses before they became too disabled to work and to return their employees to the labor force after a work-limiting disability occurs.
A third avenue of policy would focus on the development of new assistive technologies to support people with mental illness in the workplace. Such efforts would dovetail well with increased incentives for employers to deploy such technologies. Currently, a significant amount of research focuses on assistive technology for people with cognitive impairment related to dementias. Although relatively little evidence exists regarding the application of such assistive technology to supporting workers with mental illnesses, the limited research to date generally suggests that assistive technologies for people with mental illnesses are most effective for individuals after stabilization of their illness.
Recent surveys show that 90% of persons with a mental illness own more than one digital device (25). Individuals diagnosed as having a mood disorder are more likely than those with schizophrenia to own a device. About 54% of adults with mental illnesses had access to a smart phone (compared with 64% of all Americans). A recent survey found that many people with serious mental illnesses use technology to help them manage their illness (26). The survey estimated that 42% used technology to help them manage symptoms such as audio hallucinations (by using music), 37% used calendar reminders, 28% used apps for medication management, and 26% used technology to connect to peers for support. These rates of use suggest that there is
potential for new technologies to help people with mental illness remain at work and engaged. However, the technologies that have been the most useful to date have been standard apps that help in the performance of “every day” tasks. Most of the technologies that are being used are not tailored to the particular needs of people with mental illness. Investments in the development of such tailored technologies, accompanied by instruction in how to make them work for employees and firms, could facilitate integration of individuals with mental illness in the workplace.
5 Conclusions
Individuals with mental illness already face substantial challenges in the labor market. They are less likely to be employed, and they earn less on the job. Everything we anticipate about how the economy will change in the 21st century suggests that these problems will get worse, despite improved access to mental health treatment. Policymakers should turn their attention to strategies that will improve the ability of people with mental illness to enter the labor market and to retain their jobs even as their symptoms alternately increase and diminish over time. Policymakers can do so by promoting programs that more rapidly identify and engage people first experiencing mental illness, so that those with a first episode can enroll in programs that offer treatment and support and that help them obtain and hold jobs. Policymakers can help by increasing the incentives for employers to employ and retain workers with mental illness, through application of the ADA and by increasing the diffusion of long-term disability programs. Finally, policymakers can invest in the development of technologies that help offset the functional sequelae of mental illness. These policy steps will work best if they are combined, so that incentives for the development and deployment of technologies are aligned. These steps have the potential to improve the well-being of individuals with mental illness today and to compensate for the increased workplace challenges that are likely to affect this group in the future.