1 Introduction
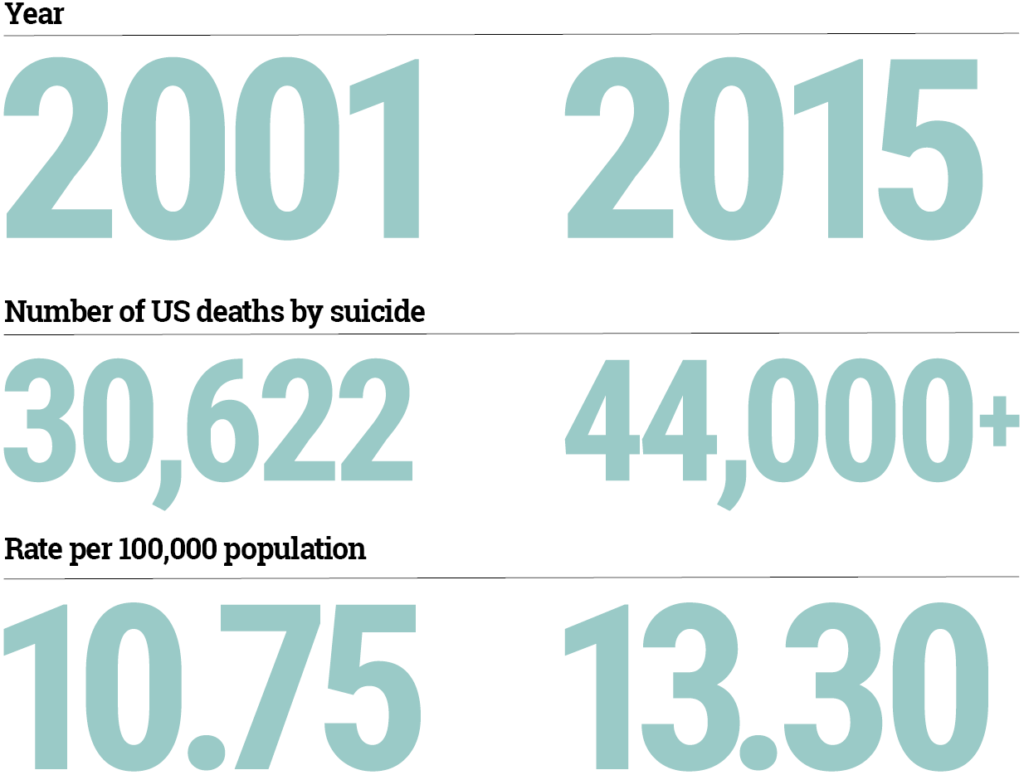
Suicide is the tenth leading cause of death in the United States, and the number and rate of suicides are rising. A brief overview of data available from the Centers for Disease Control and Prevention illustrates the increasing incidence of suicide but also suggests priorities for action. In 2001, there were 30,622 deaths from suicide (a rate of 10.75 per 100,000 population); by 2015, there were over 44,000 (a rate of 13.3 per 100,000). In addition, each year more than 900,000 emergency department (ED) visits are made by people thinking of suicide. Costs for ED visits and hospitalizations associated with self-injury among young adults alone were $2.6 billion in 2010. There are also substantial personal costs associated with suicide, as many individuals are deeply affected by suicide loss in their families or among close friends.
This white paper is intended to provide policymakers with ideas for action on suicide prevention. The emphasis is on suicide prevention among adults that is focused on improved healthcare and community prevention activities. Too many lives are lost, and we can take steps to prevent the tragedies.
2 Patterns of Suicide Suggest Priorities for Action
Suicide rates are higher for men than for women by a factor of about 3.5:1. Suicide is quite rare among young children, but rates begin to rise in adolescence (when suicide is the third leading cause of death) and rise slowly through adulthood. Men ages 35 to 64 are 19% of the population but account for 40% of suicide deaths. The increase in suicide rates among middle-aged Americans, especially white Americans, has been identified as a key contributor to increases in overall U.S. mortality rates related to economic and social challenges— sometimes labelled as “deaths of despair,” which also include drug overdoses.
These broad data suggest a need to emphasize prevention and intervention with adults in order to complement existing efforts focused on youth suicide prevention. Suicide prevention has not been emphasized in most healthcare settings, even though we know that many individuals who die by suicide were engaged in care or had recent contact with health providers. Studies have shown that about 45% of those who died by suicide saw a primary care physician in the 30 days before they died, and about 10% were seen in an emergency department in the prior two months (1,2). Thus efforts in healthcare settings to improve identification of and support to individuals troubled by suicidal thoughts are needed.
Suicide also occurs at a high rate among people receiving care in behavioral health settings. About 30% of all suicide deaths are among those who received behavioral healthcare. Indeed, the rate of suicide among individuals cared for in state mental health systems has been reported to be as high as 140 per 100,000, or ten times the national rate (personal communication, Heise J, July 28, 2016). It is clear that people with mental and substance use disorders have elevated suicide risk. However, the greatly elevated rates among people receiving care suggest that attention to suicide prevention in behavioral health services is another priority for action. The services sector that is the preferred referral destination for suicidal individuals should provide care that is “suicide safe.”
3 Evolution of the Suicide Prevention Field
The first National Strategy for Suicide Prevention was released by Surgeon General David Satcher in 2001. Before then, the most successful prevention program was a 1990s U.S. Air Force effort. The Air Force program was a broad population-based approach, emphasizing leadership, community education, improved healthcare, and surveillance. Drawing from this effort, the initial national strategy emphasized public health methods, including increasing awareness and providing better access to mental healthcare. However, implementing these approaches has been more difficult in typical communities than in the Air Force. And the challenges are daunting: resources for suicide prevention have been extremely limited, and responsibility has been diffuse.
The decade following the new 2001 strategy saw an expansion of suicide prevention efforts, including the 2004 Garrett Lee Smith (GLS) Memorial Act, which created a youth suicide prevention grant program administered by the Substance Abuse and Mental Health Services Administration (SAMHSA). The GLS program is focused solely on youth ages ten to 24, and there is to date no national suicide prevention program for adults. Most GLS grantees emphasized screening, strengthening community partnerships, and building awareness of suicide warning signs in schools and communities. Results suggest that counties implementing these activities had lower suicide attempts and deaths among youth, compared with matched counties (3). However, reductions in suicide were observed only among the target population of youth and did not persist after the programs ended. The results suggest that community-based prevention efforts can have an effect, but they must be sustained and targeted at the population of concern.
Other national efforts since 2000 include establishment of a SAMHSA-funded technical assistance center (the Suicide Prevention Resource Center) and a crisis call system (the National Suicide Prevention Lifeline). In 2007, the Department of Veterans Affairs (VA) established suicide care protocols for its facilities and now supports a national hotline for veterans in crisis that has answered nearly two million calls and dispatched emergency services for over 56,000 veterans. Evaluation of the VA efforts showed some success in preventing suicide among veterans engaged in VA services, but persistent high rates of suicide were noted among veterans not engaged in care (4).
4 Promising Practice: Making General Medical and Behavioral Healthcare Settings “Suicide Safe”
Zero Suicide is an approach to suicide prevention in healthcare. It is based on research on effective practices and an overall approach launched in 2001 by the Henry Ford Health System (HFHS) in metropolitan Detroit. The HFHS Perfect Depression Care initiative is a quality improvement effort with a goal of “zero defect” mental healthcare. The audacious goal of zero deaths by suicide is one measure established for the program. Key elements of the approach are suicide assessment for all behavioral health patients and emphases on ready access to care, means restriction, provider education, and follow-up phone calls. The HFHS program reduced the suicide rate among patients receiving behavioral healthcare from an average of 96 per 100,000 in 1999-2000 to an average of 24 per 100,000 in 2001-2010 (5). During this period, suicide rates in the overall population served by HFHS stayed level while deaths in Michigan rose.
Based on the HFHS approach and new research on effective interventions, a task force of the National Action Alliance on Suicide Prevention, a public/private guidance and advocacy group launched in 2010 by Secretaries Sibelius (Department of Health and Human Services) and Gates (Department of Defense), developed the Zero Suicide care model. An online toolkit as well as training and support for implementing organizations have been developed by the Suicide Prevention Resource Center. The approach is being implemented in several hundred organizations, and formal implementation efforts are under way in at least half the states. Preliminary data suggest that Zero Suicide is effective.
5 Next Steps in Suicide Prevention: Focused Priorities, Filling Gaps, and Building on Successes
Against the backdrop of some improved tools to fight suicide, rates have continued to rise. Increased concern coupled with improved knowledge has created an environment in which effective action is now possible. Some consensus on priorities is emerging based on work done by the National Action Alliance on Suicide Prevention.
Importantly, increased concern about suicide led to commitments in the 21st Century Cures Act. The act reauthorized existing programs (the National Suicide Prevention Lifeline, the GLS Memorial Act, and the Suicide Prevention Resource Center) and also authorized a national effort focused on adult suicide prevention and an effort to improve crisis intervention services. Crisis services—both hotlines and programs such as mobile crisis teams—are integral to suicide prevention. Until recently, specific crisis care interventions, such as ED visits, have been reimbursed by some health insurance programs, such as Medicaid, but aside from minimal national support for the National Suicide Prevention Lifeline (and the VA’s crisis line), there has been no federal support for the necessary infrastructure of crisis systems. The commitments included in the 21st Century Cures Act have not yet been advanced by appropriations, but they represent an initial national commitment to suicide prevention that can reach beyond the time-limited grants to a few communities.
Alignment on Priorities
Congressional interest and action, coupled with growing national concern and increased knowledge about suicide prevention targets and approaches, set the stage for action. However, selecting and advancing responsive strategies remains important. In this context, a new national approach offers promise. The National Action Alliance on Suicide Prevention has recently joined with the American Foundation for Suicide Prevention (AFSP) to announce an initiative to reduce suicide rates by 20% by 2025. Targets for the effort were chosen based on modelin g the impact of selected projects deemed high impact and feasible. Importantly, the priorities align well with legislative targets included in the 21st Century Cures Act. The Action Alliance/AFSP initiatives include:
Accelerating adoption of better suicide care (also known as Zero Suicide) in healthcare settings, especially in large healthcare systems.
Improving suicide screening, brief interventions, and follow-up to individuals seen in emergency departments.
Collaboration with the firearms industry to provide suicide prevention education to individuals who purchase a firearm.
We will not succeed in preventing suicide unless we know more about what leads individuals to take their own lives and until we have developed new and effective prevention strategies.
The firearms safety initiative was developed by AFSP with the National Shooting Sports Foundation, based on projects in New Hampshire and other states. The effort has already been planned and announced, with an implementation plan in place. Given this promising development plus the contentious nature of firearms issues, the project should proceed with support of suicide prevention advocates. On the other hand, because of the ambitious nature of orienting healthcare to suicide prevention, more work is needed to advance this priority. Finally, achieving the promise of the newly authorized (but not yet funded) suicide prevention and crisis intervention priorities of the 21st Century Cures Act requires advocacy and modest appropriations.
Implementation Strategies to Advance the Suicide Prevention Priorities Improving suicide care in healthcare settings is timely. Until very recently, suicide prevention was not defined as a core responsibility of either behavioral healthcare or general medical care by mainstream quality improvement or patient safety organizations—except for inpatient settings. However, in 2016, The Joint Commission signaled a new focus on suicide prevention by releasing a new Sentinel Event Alert; its aim is to “assist all healthcare organizations [emphasis added] providing both inpatient and out-patient care to better identify and treat individuals with suicidal ideation” (6). Coming from the leading accreditor of hospitals, the alert is a significant step toward establishing suicide prevention as a healthcare priority and provides support for the Action Alliance/AFSP initiatives focused on large health systems and EDs. However, the infrastructure and incentives to motivate adoption of suicide safe care are not yet adequate to support rapid, large-scale adoption.
Action recommendation:
The federal and state governments as well as accreditors and patient safety organizations should consider adopting clearer requirements for suicide-safe care in healthcare organizations, and they should support development of the infrastructure needed to implement these requirements.
This priority is closely related to the actions and initiatives needed to bring to life the promise of suicide prevention efforts in the 21st Century Cures Act. An explicit focus on preventing suicide among adults—especially men in the middle years—is necessary given its high burden. It is now feasible because of the synergy with efforts across the healthcare system and because strategies for community efforts that complement healthcare projects have been demonstrated to be successful for youth and developed by several Action Alliance task forces (for example, the Faith Communities Task Force).
Action recommendation:
Advocates should urge, and Congress should enact, the modest appropriations needed to develop a national suicide prevention initiative for adults incorporating community-based social service and educational elements and healthcare elements.
The effort to build an adult suicide prevention approach should be led by SAMHSA in partnership with the National Institute of Mental Health, which must provide relevant research support. However, participation by other federal, state, and local partners is essential. Partnership with criminal justice authorities is important, because the burden of suicide is high among people involved with law enforcement and the criminal justice system.
The remaining new commitment related to suicide prevention in the 21st Century Cures Act is authorization of funds to SAMHSA to support crisis programs, beyond the small appropriation for the National Suicide Prevention Lifeline. The roughly $7 million appropriation for the lifeline supports its national infrastructure, but most crisis calls are answered through a network of local and statewide call centers. Many calls cannot be answered in the region or even the state where the call originates, because crisis lines in that area are not adequately funded. In addition, even in communities where call center capacity is sufficient, resources to provide more than a phone call (for example, a visit by a mobile crisis team, a brief stay in a crisis stabilization facility, or real-time inventories of available crisis and inpatient beds) are not present.
The absence of a crisis care infrastructure also results in thousands of expensive psychiatric hospital admissions that would not be needed if other options were present. This misuse of resources also means that inpatient beds may not be available for people in distress from serious and acute mental illness, for whom a brief hospital stay may be very helpful.
Action recommendation:
Advocates should urge, and the Congress should enact, the modest appropriations needed to begin to develop a national mental health crisis response infrastructure.
This initial step requires only a very modest investment but is perhaps the most crucial step that can be taken to reduce the overreliance on law enforcement to do mental health work and to address the practice of “psychiatric boarding” in which people with mental illness are detained for many hours—or in some cases days, or even weeks—in inappropriate care settings.
6 Conclusions
The emphasis of these policy prescriptions is on research and education. We will not succeed in preventing suicide unless we know more about what leads individuals to take their own lives and until we have developed new and effective prevention strategies. Public education is also central to preventing the tragedies associated with suicide. Following the policy recommendations outlined in this white paper will help to prevent suicide and avert its tragic consequences.
Public education is central to preventing the tragedies associated with suicide.