1 Medicaid: The Nation’s Health Insurance Program for Low-Income People
Medicaid is a federal-state health insurance program for poor and low-income individuals. Medicaid enrollees generally have more complex health needs than the general population, and the Medicaid program serves as a safety net for many low-income individuals who have limited options for obtaining health insurance coverage. The program plays a particularly important role in providing coverage for people with mental and substance use disorders. The focus of this paper is on the implications of proposed policy changes in Medicaid for those individuals.
Before passage of the Affordable Care Act (ACA), individuals generally were eligible for Medicaid only if they met income requirements and also fell into an eligibility category of covered persons, such as parents of dependent children or individuals with disabilities. These rules excluded many low-income adults without dependent children who had complex health needs but did not meet criteria for having a disability. Low-income individuals who were historically ineligible for Medicaid were more likely to be males, non-Hispanic whites, older than age 45, living in the South, and slightly healthier than the Medicaid-eligible population (1). Because they were ineligible for Medicaid coverage and had limited access to other types of coverage, many of these people remained uninsured.
Under the ACA, states may now expand Medicaid eligibility to include almost all adults at or below 138% of the federal poverty level (FPL), or $27,821 for a family of three in 2016. States receive enhanced federal funding to finance the cost of this expansion. As of January 2017, 31 states and the District of Columbia had expanded Medicaid, (2) and 11 million adults had gained coverage under these expansions (3).
2 Medicaid’s Current Role in Behavioral Healthcare
Medicaid is a major source of health coverage and financing for behavioral healthcare in the United States. The program covers a disproportionate share of individuals with behavioral health conditions: in 2014, 20% of adults with any mental illness, 24% of adults with serious mental illness, and 16% of adults with a substance use disorder were covered by Medicaid (Figure 1) (4). For comparison, 12% of adults in the general population were covered by Medicaid.
Medicaid’s behavioral health benefits are generally more comprehensive than those provided by other payers (5) and include not only acute care services but also long-term services and supports to enable many people with chronic illness to receive community-based versus institutional care. Some of these services are mandatory services (e.g., hospital services and psychiatric treatment) that all states must cover under federal law. However, many services, such as case management, prescription medication, and rehabilitative services, are provided at the option of the state. Flexibility in Medicaid benefits coverage enables states to cover non-clinical behavioral health services, including those that have emerged as evidence-based practices for treating individuals with the greatest impairments (e.g., assertive community treatment), and to adapt to changing patterns of care, such as the demand for medication-assisted treatment of opioid use disorder.
Medicaid expenditures for behavioral health are significant, both in terms of overall Medicaid spending and in terms of national spending for behavioral healthcare. Nationally, Medicaid funded 25% of all mental health spending and 21% of spending for treatment of substance use disorders in 2014, (6) and in 2011, enrollees with behavioral health conditions accounted for 48% of Medicaid spending (7). Numerous studies have documented that Medicaid expansion under the ACA has had positive effects on behavioral health services in states that expanded, including increases in availability of and access to behavioral health services (8,9), decreases in unmet need for behavioral health services among low-income adults (10), better integration of behavioral health and primary care (11), increases in mental health services and staffing at safety- net facilities (12,13), and state savings from enhanced federal matching funds, particularly in behavioral health programs (14).
In recent years, state Medicaid programs have also made strides in scope of benefits and service delivery models in behavioral health, often using state flexibility to design and test new approaches to care. Federal parity rules require Medicaid managed care organizations (which deliver care to the majority of Medicaid beneficiaries) (15) to cover behavioral health services at parity, which means that behavioral health services must be covered to the same extent as general medical services. Parity rules apply to several aspects of behavioral health treatment, including cost-sharing, deductibles, and treatment limits (16),with the goal of making behavioral health services accessible and affordable for Medicaid beneficiaries who would otherwise be unable to obtain care.
Medicaid also has undertaken many service delivery changes that have made behavioral healthcare more accessible and effective. For example, over a third of states (20 states) have taken advantage of the “health homes” plan option in Medicaid (17), which enables states to better coordinate care for enrollees with chronic conditions. Most Medicaid health home programs include beneficiaries with behavioral health conditions (primarily serious mental illness) (18), and through this benefit, providers can integrate and coordinate physical health, behavioral health, and long-term services and supports for enrollees. Other Medicaid programs have implemented other strategies to better integrate physical and behavioral healthcare, including universal screening for both physical and behavioral health conditions and the co-location of services at one facility (19). Some states have expanded the availability of community-based services to help people with mental illness transition out of institution-based care (20).
Fig. 1 Medicaid Coverage Among Adults with Behavioral Health Conditions, 2014
Share with Medicaid:
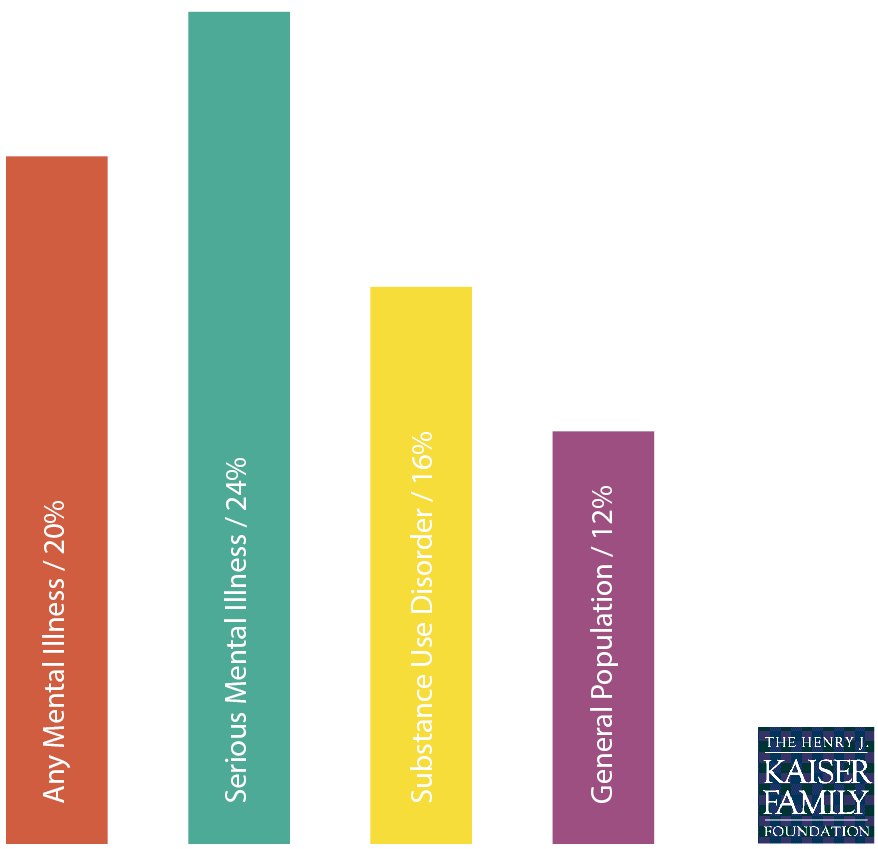
Source: Kaiser Family Foundation analysis of National Survey on Drug Use and Health, 2014
3 Proposed Changes to Medicaid and Implications for Behavioral Health
Recent proposals for health reform have called for fundamental changes to the current Medicaid program, including repealing the ACA (including the Medicaid expansion) and restructuring federal Medicaid financing. Although the potential effects of these proposals are difficult to predict without more specific information about their implementation, it is very likely that these changes would lead to coverage losses or barriers to access for many people with behavioral health needs. The changes also could lead to decreased federal funding to states to finance and deliver services to residents with mental and substance use disorders, increasing the burden on states at a time when systems are already stretched by a growing opioid misuse crisis.
Repeal of the ACA Medicaid Expansion
The specific effects of ACA repeal would depend on many factors, including which provisions are repealed and whether a replacement plan is provided. However, some estimates project that if the expansion is repealed, an estimated 1.3 million people with serious mental disorders and 2.8 million people with people with substance use disorders would lose some or all of their insurance coverage (21). Although some of these people may be able to qualify for the traditional Medicaid program on the basis of having a disability, the process of gaining eligibility through this pathway requires a difficult and lengthy determination, during which individuals may lose coverage for significant amounts of time and may experience worsening symptoms as their conditions go untreated. Furthermore, individuals in the early stages of a potentially disabling condition, who do not yet meet criteria for disability under the Supplemental Security Income (SSI) program, could lose coverage for early intervention services that might forestall entry onto the SSI rolls. Although some individuals who gained coverage during the Medicaid expansion could have qualified for SSI and Medicaid prior to the expansion, qualifying for Medicaid based on income alone allows enrollees to obtain coverage more quickly and seamlessly (22), which likely encouraged many of these individuals to finally obtain the coverage for which they had been eligible for a long time.
Repeal of the Medicaid expansion has implications beyond reductions in Medicaid enrollment. A large body of literature demonstrates that Medicaid coverage helps facilitate access to needed care (23). Thus loss of coverage could lead to decreased access to early intervention and treatment services for behavioral health conditions, which are essential for improving health outcomes. In addition to affecting health outcomes, untreated behavioral health conditions are associated with increased societal costs, which come from greater reliance on the emergency room, greater involvement with the criminal justice system, and loss of productivity resulting from being unable to work (24,25,26,27). Loss of coverage also has potential negative consequences for behavioral healthcare providers, many of whom changed their operations in response to the ACA, for example, by accepting Medicaid and other insurance for the first time, and who saw a significant decline in uncompensated care costs under the ACA (28).
Waivers to Impose Work Requirements
Other reform efforts are focused on use of Medicaid waivers for states to modify their programs. Medicaid waivers provide states an avenue to test new approaches that differ from federal program rules; waivers can provide states considerable flexibility in how they operate their programs, beyond what is available under current law. Existing waivers include provisions not otherwise permitted under current Medicaid rules, such as premiums, co-payments above statutory limits, healthy behavior incentives, or the provision of premium support for purchasing private coverage (29).
Although the previous administration did not approve waiver requests to impose work requirements for Medicaid, recent policy statements have indicated interest in imposing work requirements (30). These requirements may pose significant challenges to Medicaid enrollees with behavioral health conditions, many of whom would struggle to pay premiums or purchase private coverage or whose disabilities may preclude them from working. Furthermore, Medicaid rarely provides full coverage of supported employment, which is an evidence-based practice shown to increase employment in competitive jobs; without this benefit, people with behavioral health problems could face challenges complying with work requirements.
Changes in Federal Medicaid Financing
In addition to repealing the Medicaid expansion, some policy-makers also have proposed changes in Medicaid financing that could limit federal financing for Medicaid through a block grant or a per capita cap. Under current law, eligible individuals have an entitlement to coverage and states are guaranteed federal matching dollars with no pre-set limit. The proposals under consideration could eliminate both the entitlement and the open-ended match to achieve budget savings and to make federal funding more predictable. To achieve budget savings, federal funding limits would be set at levels below expected levels if the current law were to stay in place. In exchange for these federal caps, proposals could allow states to impose enrollment caps or waiting lists or reduce eligibility levels or offer states other increased flexibility to design and administer their programs. Many proposals do not specify the rules for whether state matching payments are required or which core federal eligibility and coverage standards would be changed.
Changes in the federal government’s terms of contributions to the Medicaid program could result in substantial limits to federal funds available to states to help them cover and finance behavioral health services. For example, the Medicaid changes in the 2016 House Budget included cuts of about 40% (including the ACA repeal and Medicaid caps in federal spending) over a ten-year period (31). Although states could gain new flexibility under these plans, it is not clear what actions states could take to preserve benefits and enrollment that they cannot already do under federal Medicaid law (32). Medicaid spending is already relatively low (largely due to lower payment rates to providers )(33). Between 2000 and 2011, Medicaid spending grew at rates below rates for private health insurance spending and national health expenditures (Figure 2). Faced with more limited federal dollars, states will face incentives or pressure (due to limited budgets) to maximize the limited federal funding they receive. As a result, they may eliminate or freeze enrollment (particularly likely under a block grant) or trim benefit packages to lower per enrollee spending (likely under per capita caps).
The implications of changes to federal Medicaid financing for behavioral health-care depend largely on design choices, but given the relatively high cost in the population with behavioral health needs (34) and the high share of Medicaid program spending for behavioral health, it is likely that such populations or services would be a target for cuts. Cuts to enrollment that affect individuals with behavioral health needs could ultimately shift these costs to State Mental Health Agencies, which bear responsibility for financing services for people with no source of coverage. Cuts to services considered ancillary, such as peer support, non-emergency transportation, non-clinical services, and prescription drugs, could have significant implications for individuals with behavioral health conditions, who rely heavily on many of these services. In particular, pressures to cut spending on prescription drugs would disproportionately affect behavioral healthcare, because central nervous system agents, which include psychiatric medications, are the largest class of prescription drugs, both in terms of total number of prescriptions and total spending (35). In addition, cuts to provider payments could hinder provider participation in Medicaid, which would exacerbate the already limited availability of behavioral healthcare providers who accept Medicaid.
Finally, financing proposals under discussion could limit states’ ability to develop new models of care, respond to emerging health issues, or respond to changing economic conditions. If federal funding is capped (either globally or on a per person basis) and limited to a pre-set growth rate, it will not change in response to unforeseen events. Medicaid’s open-ended financing has enabled it to respond to recent events, such as the Great Recession, which saw an uptick in mental distress, (36) or the recent opioid crisis. This ability to address emerging needs has made the Medicaid program a key component of the nation’s response to behavioral health crises.
Fig. 2 Average Annual Spending Across Medicaid and Other Benchmarks, 2000-2011
Average Annual Growth Rates, 2000-2011
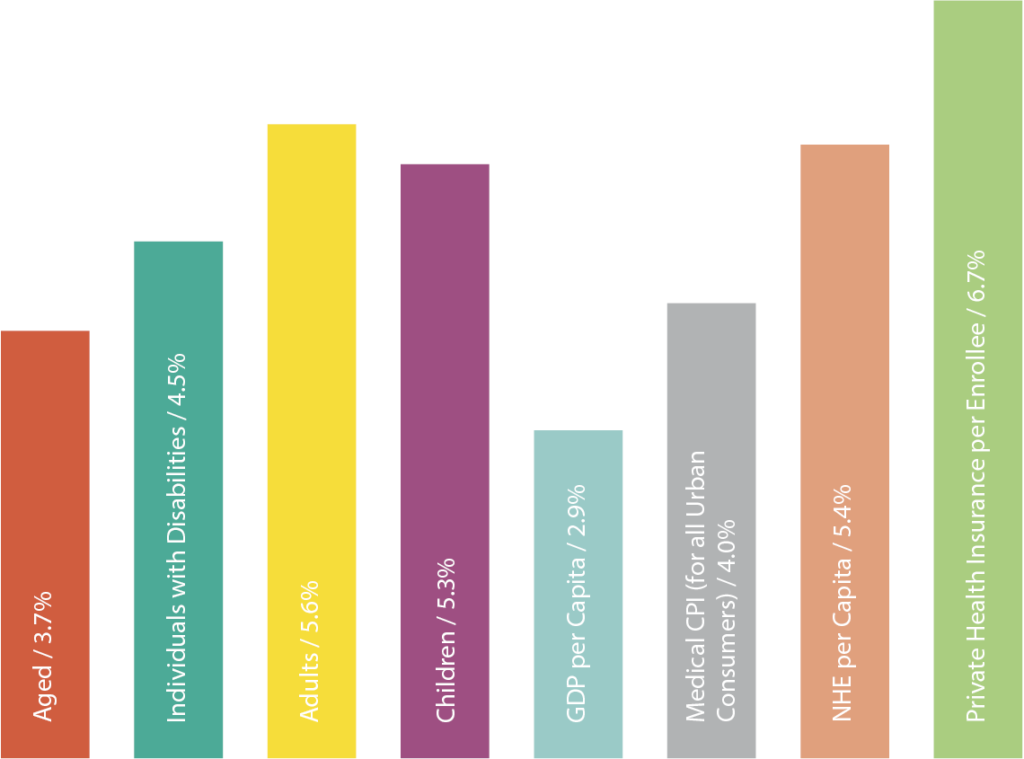
Note: Growth rates by Medicaid eligibility groups are for fiscal years 2000-2011. Source: Growth rates by eligibility group from KCMU and Urban Institute estimates based on data from FY 2000, 2001, 2010, and 2011 MSIS and CMS-64 reports. GDP per capita from The World Bank National Accounts Data, available at http://bit.ly/2mAnoZ3. NHE per capita and Private Health Insurance per enrollee from the National Health Expenditure Accounts, available at http://go.cms.gov/2nR9amP. Medical CPI-U growth from Bureau of Labor Statistics, available at https://www.bls.gov/cpi/
4 Conclusions
Medicaid has been an important resource for many low-income individuals with behavioral health conditions. Recent policy changes, including Medicaid expansion, federal parity rules, and service delivery changes, have further facilitated access to care. However, the proposals to repeal the Medicaid expansion and limit federal financing for Medicaid through a block grant or a per capita cap have important implications with regard to eligibility, coverage, access, and costs. When evaluating the potential impact of these proposals, it is important to be mindful of the unique and complex needs of enrollees with behavioral health conditions, as well as the ways these proposals will affect the providers and systems that care for them.
When evaluating the potential impact of these proposals, it is important to be mindful of the unique and complex needs of enrollees with behavioral health conditions, as well as the ways these proposals will affect the providers and systems that care for them.


